THE BACTERIUM: Staphylococcus aureus is a natural bacterium in human hosts that can also cause a broad spectrum of disease. Populations that are reported to have increased risk of S. aureus colonization includes those with type 1 diabetes, intravenous drug users, asthmatic patients, the elderly, those with rheumatoid arthritis, and chronic sinusitis sufferers. Factors that can increase the potential for colonization include poor personal hygiene and sharing of personal items. The risk of outbreak is increased in groups who share spaces such as military barracks, day care facilities, and locker rooms.
One study assessed the colonization of S. aureus in 377 athletes and athletic trainers and reported the prevalence of MRSA ranged anywhere from 8% to 62%, depending on time of assessment. Most publicized reports of CA-MRSA infections in athletics have been on college or professional football teams, but wrestling, rugby and fencing have also reported cases of CA-MRSA.
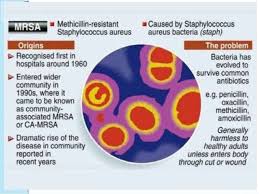
HA-MRSA v. CA-MRSA: Over the last 4 decades there has been an escalation in not only healthcare-associated methicillin-resistant S. aureus (HA-MRSA), but community-associated MRSA (CA-MRSA). CA-MRSA infections have become more common in athletes since the first reported cases in 1993 and 1998. A study of all Nebraska high schools between 2006 and 2008 (Buss, et al) determined that MRSA infections rose from 4.4% to 14.4% over that period; Per 10,000 football players it increased from 5.0 to 25.1. Additionally, the incidence per 10,000 wrestlers rose from 19.6 to 60.1.
CA-MRSA differs from HA-MRSA in its genetic makeup and its susceptibility to antibiotic treatment. CA-MRSA has been found in certain cases to be more virulent than HA-MRSA. CA-MRSA has been associated with furunculosis and bone/joint infections, but most commonly presents as a skin infection as the result of an abrasion (i.e. turf burns) or laceration. Skin and soft-tissue infections (SSTIs) represent nearly 90% of all S. aureus infections; this includes folliculitis.
SIGNS & SYMPTOMS: Most often an athlete might describe a CA-MRSA SSTI as an “infected pimple” or “insect bite”. Depending on severity, some CA-MRSA infections may progress to an abscess. Other signs and symptoms include:
• Bump that is painful, red, leaking pus and/or swollen
• Bumps under the skin that are swollen or hard to the touch
• Skin around a sore that is warm or hot to touch
• Bump that grows rapidly and/or does not heal
• Painful sore accompanied by a fever
• Rash or pus-filled blisters
• Draining boil or bacess
MODES OF TRANSMISSION IN ATHLETICS: The most common mode of transmission of CA-MRSA is through an open wound, including an abrasion or laceration. Other modes include poor hand washing, poor personal hygiene (such as not showering after workouts), sharing personal items (razors, towels, clothing) or failure to properly clean and disinfect exercise equipment.
The sports most susceptible to the spread of CA-MRSA are those with lots of physical contact: football, wrestling, rugby, but they have been reported in other sports including soccer, basketball, field hockey, volleyball, rowing, martial arts, fencing and baseball.
TREATMENT & MANAGEMENT: Depending on the severity of the infections, treatment can be given on an outpatient or inpatient basis. For outpatient treatment, the most common method includes topical and/or oral antibiotics. The most commonly prescribed oral antibiotics include Trimethosprim-sulfamethoxazole, Clindamycin, Doxycycline and Linezolid. As needed, abscesses will be drained; drainage will then be sampled and tested to confirm MRSA as appropriate.
Moderate to severe CA-MRSA infections could require surgical debridement of the abscess, intravenous (IV) antibiotics and hospitalization, as needed. The most commonly used IV antibiotics included Vancomycin, Linezolid, Clindamycin, Daptomycin, Ceftaroline, Dalbavancin, and Tedizolid.
RETURN TO PLAY: Athletes with mild cases of CA-MRSA should be withheld from participating in team activities for at least72 hours (3 days) after starting oral antibiotic therapy in combination with the presence of a well-formed scab without an active discharge. All abrasions should be covered, infected or not and the athlete’s healing progress should be monitored daily for recurrence of infection or the development of new infections.
To ensure infection is not transmitted to others according to the Centers for Disease Control in addition to ensuring the infected wound is covered athletes should clean their hands often, but especially after changing the bandage(s). It’s especially important not to share towels, washcloths, razors and clothing. Following washing and drying instructions for laundry, ensuring clothing is completely dry is also critical.
PREVENTION: The key to prevention of CA-MRSA is proper hygiene including regular hand washing using warm liquid soap (not bar soap) and water. The use of bacterial hand gels should be included too. Athletes should be educated on these hygiene procedures as well as not sharing personal hygiene items including razors or towels. Additionally, open wounds should be properly managed and covered – do not pick or pop anything that looks like an infected pimple, if infected, it will spread the infection.
Athletic trainers and equipment and facilities managers are also critical to the prevention of CA-MRSA. Cleaning locker rooms, wrestling mats, athletic training tables and whirlpools with a proper disinfectant helps minimize the spread of MRSA as well as using universal infectious disease precautions when treating athletes. Proper disposal of potentially infected dressings is also important Equipment managers should also be sure to use appropriate laundry cleaning procedures to minimize the spread through towels and athletic uniforms, including ensuring clothes are dried completely.
The CDC provides a specific resource for the Prevention of MRSA in Athletic Facilities.
Disclaimer: The content contained in this blog is for informational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician, athletic trainer, or other qualified health provider with any questions you may have regarding a medical condition. If you think you may have a medical emergency, call your doctor or 911 immediately.
PRIMARY RESOURCE: MRSA Skin Infections in Athletes (2017)
OTHER RESOURCES:
CDC MRSA Prevention Information and Advice
Stanford Children’s Hospital Preventing MRSA in Athletics
Infectious Diseases Associated With Organized Sports and Outbreak Control (2017)
NATA Position Statement: Skin Diseases
Common Dermatologic Infections in Athletes and Return-to-Play Guidelines (2011)

